Baby-Friendly Changing Lives in Rural Mississippi
Sunflower County, Mississippi, is not a place where one would expect to see rapid social change. Home to roughly 30,000 people in rural Mississippi, it is steeped in its heritage and traditions.
Yet, in the past few years, families in Sunflower County have witnessed a revolution of sorts – at least as it relates to the experiences of new mothers and their babies in the precious first days of life – thanks to the advent of Baby-Friendly practices at the county’s only birthing facility, South Sunflower County Hospital, located in Indianola, Mississippi.
An Insurer’s Perspective

Sarah Broom, MD, is Medical Director for BCBSMS and a strong advocate for Baby-Friendly practices and other evidence-based maternity quality measures.
“The evidence shows that breastfeeding is linked to improved outcomes,” she says. “We have some serious healthcare issues in our state – childhood obesity, diabetes, maternal morbidity and mortality, breast cancer – and we knew increased breastfeeding could have a positive impact in these areas. So, our management made the bold and important decision that we were going to encourage a commitment to the Baby-Friendly Hospital Initiative among our network hospitals.”
Read more about Sarah’s experience
A Task Force Leader’s Perspective

Betsy Dawson, CFNP, led the Baby-Friendly Task Force for the hospital.
“Educating moms on breastfeeding and taking care of their babies is a passion of mine,” she says. “When Blue Cross & Blue Shield of Mississippi discussed Baby-Friendly with us, along with the opportunity to work with CHAMPS, of course, we jumped on it. This is the town where I was raised and this is the town where I’m raising my children. I wanted to do everything I could to encourage this and educate our moms here.”
Read more about Betsy’s experience
A Proud Moment for the Hospital
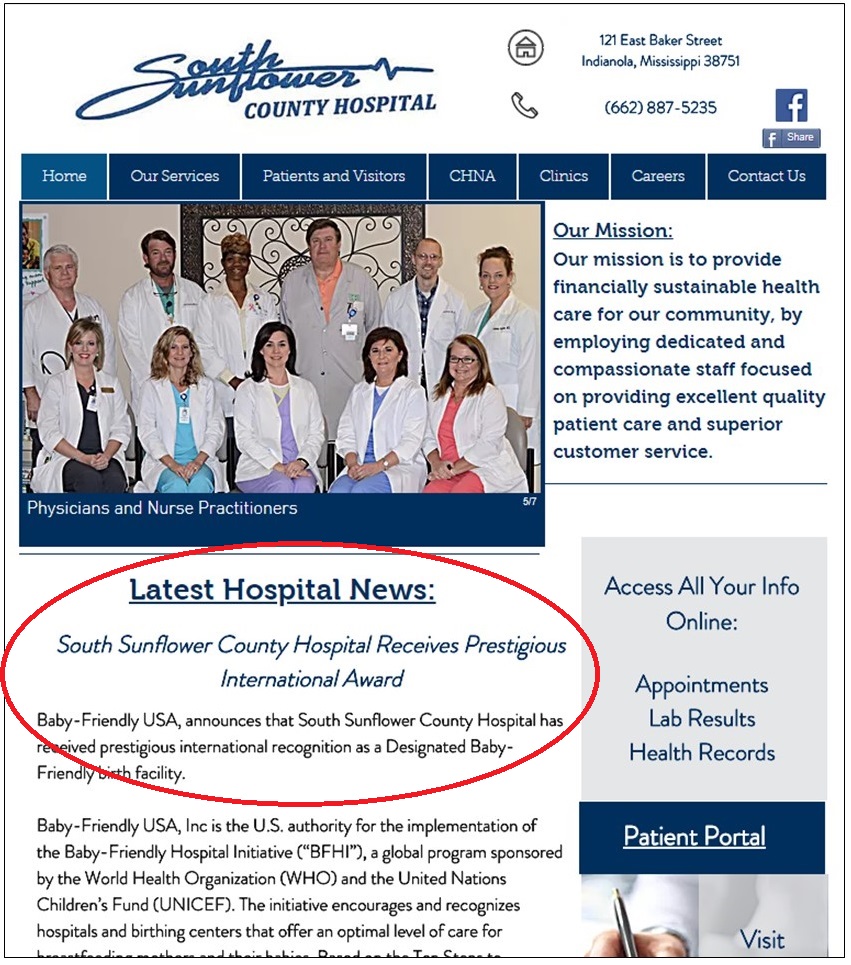
As Baby-Friendly USA approaches the once seemingly unattainable milestone of 1,000,000 babies born each year in Baby-Friendly facilities in the US, South Sunflower’s approximately 300 births per year may seem like a drop in the ocean. But the dedicated professionals who work in the hospital’s maternity ward believe Baby-Friendly practices are helping to change their world.
A Frontline Nurse’s Perspective

“Down the road, I think we’re going to see a closer family, a closer-knit mother-child bond,” she says. “We have grandmothers and extended families taking care of babies and moms don’t have the attachment with their babies. I think this will bring moms closer to their children. We’re going to see more maternal attachment and we’re going to see the family come back in our community.”
Read more about Jennifer’s experience
A Mother’s Perspective
These sentiments are echoed and the changes are much appreciated by South Sunflower’s recent patients.

“I really loved it the second time because I didn’t have to worry about what was going on when he was away from me – because he was never away from me. I really liked that,” she says. “I was also more educated on what to expect when it came to breastfeeding and I really wanted to breastfeed. So, I felt more comfortable doing it from the get-go.”
Read more about Tina’s experience

“After I had her, they asked me, did I want to try to breastfeed,” she says. “I said no, I wanted to bottle feed. But she didn’t take to the bottle. We tried for two days to get her to take the bottle. So, they said again, why don’t you try your breast. The moment I tried it, she latched on, no problem. It’s like she knew what she wanted. So that’s how I ended up breastfeeding. Everything I needed to know about breastfeeding, they helped me 100 percent. I’m glad I did it because there’s a lot of benefits from it.”
Read more about Tiesha’s experience
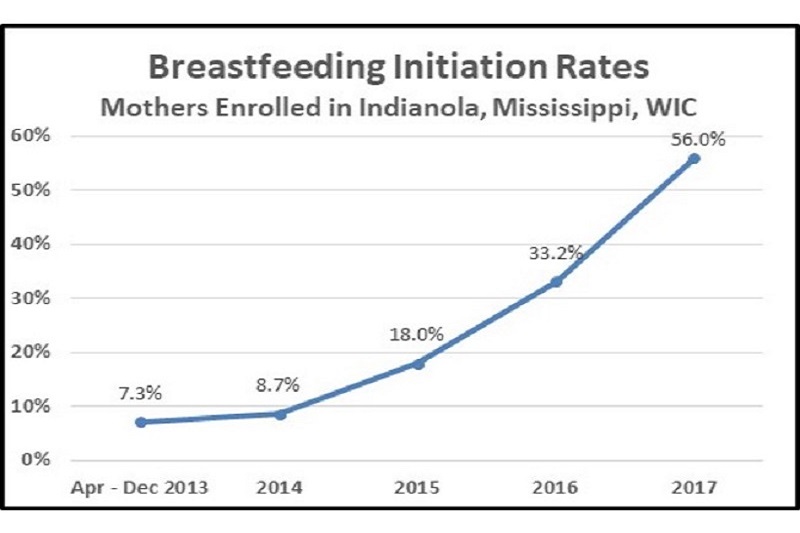
A Changing Culture
Before and After Baby-Friendly: An Insurer’s Perspective
Sarah Broom, MD

What was the motivation to get this started?
“About five years ago, it was very clear to us that it was important for maternity care in general to improve in Mississippi. Looking at infant and maternal data as far back as the 90s, it was easy to see that we had room for improvement. It was important to our management to begin to create a structure by which maternity care could improve in the state. And so, we began to develop a Maternity Quality Model. This model has multiple components, one of which is Baby-Friendly Hospital Initiative implementation (BFHI) in all delivering Network Hospitals.
“We began to work with the Mississippi Perinatal Quality Collaborative, and of course, among their goals were to improve infant outcomes and to improve breastfeeding rates. And so, management made the decision that we were going to do more than encourage breastfeeding, we were going to encourage a commitment to the BFHI because it is about patient education and employs evidence-based practices.”
Can you talk more about the link between breastfeeding and the improved outcomes you seek?
“In 1996, the infant mortality in Mississippi was 11 (per 1000 births). In 2016, it is 8.6. Also, the infant mortality in the poorest counties in the state – Tunica, Coahoma, Sunflower – has dropped. The evidence shows that breastfeeding is related to improved outcomes. We have some serious healthcare issues in our state – childhood obesity, diabetes, maternal morbidity and mortality, breast cancer – and we knew increased breastfeeding could have a positive impact in these areas.”
What appeals to you most about Baby-Friendly practices?
“The BFHI is about relationships. It’s about the mother’s relationship with baby – the opportunity to have as much skin-to-skin time and experience learning to care for her baby as possible during her time in the hospital as a result of rooming-in. It’s about relationships between the hospital care team and the mother and baby. It’s also about the relationships among hospital care team members – because there’s a breastfeeding policy in the hospital that every team member understands and follows as well as a method of charting and a method of educating. It’s a paradigm change, and it’s all about relationships in the hospital.
“It’s also about parenting. If you’ve got this baby in the room with you for 48 hours and you’ve never seen a baby before or held a baby before, it’s reassuring to know that someone is there to teach you how to bathe her, feed her and how to safely position her for sleep. It’s about more than just having a baby and getting a car seat. Baby-Friendly fosters a lot of caregiving. It’s a paradigm change in the woman’s hospital experience that allows her to form a relationship with her baby and gives her the ability to make informed choices about feeding her baby.
“Ultimately, it’s about patient education. Not everybody goes home breastfeeding. Not everybody who goes home breastfeeding continues to breastfeed. But with the BFHI, we know that every mother is educated and has the opportunity to make an informed choice about breastfeeding. She can decide not to, but she gets the support and information she needs to make that choice – which she wasn’t necessarily given before. That’s what we want to send her home with – more knowledge. We want her to get more knowledge when she’s at home… more knowledge before she delivers… and, ideally, more knowledge before she conceives.”
Could you talk more about the paradigm shift for hospitals?
“I remember when a nurse manager from one of our hospitals that has achieved Baby-Friendly status said, ‘You know, this used to be our baby. Now we realize this is not our baby. This is the parents’ baby. And we need to support them in caring for and getting to know their baby.’ This goes to the whole healthy start idea of family resilience and family support.”
Do you ever get people pushing back saying they’re just doing this to save money?
“We as humans don’t like change. Change is hard. Learning is hard. Quality is hard. What we’ve tried to do is make learning exciting. That’s why we’ve partnered and collaborated with CHAMPS. We believed in their model because it is so supportive of the hospitals, helps the learning make more sense and makes it more practical. They give such great instruction on data collection, assistance on the breastfeeding policy and the educational components of the 10 Steps.”
What do you say to people who question the efficacy of Baby-Friendly practices?
“This is about quality, evidence-based practices and giving a mother the opportunity to make an informed choice. It’s not dictating to a mother what she’ll do. The BFHI is about giving a woman an opportunity to know what she can do if she chooses breastfeeding and what she can do if she chooses bottle feeding or something in between. It’s all about informed choice and having support for whatever choice that is. I’m sure there are plenty of woman who embrace skin-to-skin and rooming in and then don’t end up breastfeeding. And that’s fine. This is not an all-or-none phenomenon. It’s a process of educating and empowering mothers to bond with and care for their babies.”
Before and After Baby-Friendly: A Task Force Leader’s Perspective
Betsy Dawson, CFNP

Can you tell us a little about your background?
“I’ve been a nurse for 14 years now. I started out as an OB nurse, which was my love, and worked there for about 4 years. Then I went back to school, got my masters, and have been working as a family nurse practitioner for 7 years now. Pregnant moms, newborns have always been my love. Educating moms on breastfeeding and taking care of their babies is also a passion of mine. So, when Blue Cross & Blue Shield discussed Baby-Friendly with us, along with the opportunity to work with CHAMPS, of course, we jumped on that. And the physicians asked me to be the task force leader.”
What made your hospital leaders convinced this was the right thing to do?
“Well, of course we all want healthy babies, healthy children, healthy adults. And if you look statistically, a breastfed baby is going to be much healthier than a formula fed baby – decreases in obesity, hypertension, cancers, the list goes on and on. I can see the difference in the babies that are breastfed and I know how much healthier they will be in the long-run. Hopefully when these babies are adults, we’ll have a lower instance of these diseases. Hopefully in 15 or 20 years, we’ll have a healthier state.”
And what made you personally motivated to achieve Baby-Friendly?
“I was definitely excited about it because this is the town that I was raised in and this is the town I’m raising my children in. And of course, the state. So, I wanted to do everything I could to encourage this and educate our moms here. It is a passion of mine.”
Could you explain the process you went through for the hospital?
“The first thing that I did was come up with a task force group. It had physicians, nurses, OB nurses, a lactation consultant from the health department, myself, and nursery workers. All the different areas. Our CEO was strongly behind this. He encouraged us, wanted us to do this. So that was great. We enrolled in CHAMPS. They helped us break it down. I could have done it without them, but it would have been really difficult. They were fantastic.
“So we first started looking at education documents. You know, the majority of this is education and support. Educating these moms, educating the family and supporting them – either way they go. We never want to push them to do it, but with just giving them education, it’s amazing the response. I came up with a packet. I didn’t want to overwhelm them, so I grouped them together and each visit, they would get maybe two pieces of paper. And the nurse would go over it and they’d talk about it and any questions. And then when she came for the next visit, we’d go on to the next section. And so, every visit throughout her pregnancy, she had some education on breastfeeding, the benefits of breastfeeding, skin-to-skin, rooming in, how to take care of your baby. Some of the basic things so then they would be prepared when they got into the hospital for what would happen.”
And that kind of thing didn’t happen before? Or it was just not organized as well?
“It was not organized and it didn’t happen unless it came from the physician.”
What about internal education for staff?
“We had in-services where they watched a video regarding Baby-Friendly hospitals and what it meant. I did in-services from housekeeping to dietary to front desk. I didn’t want anybody to not know about Baby-Friendly and what it was.”
Were there any resisters or naysayers?
“There were a few, but not nearly as much as I thought. But, you know, if that’s their opinion, then I’ll them have their opinion and they’re entitled to that…and you know, just keep on going.”
And what about moms who say they don’t want to breastfeed?
“It’s OK, but we’re still going to have a discussion with you. It’s not just about breastfeeding. Any questions and we’ll support you either way. But just know that we’re there for you if you do want the breastfeeding. And a lot of times, they end up in the end wanting to try. It may not be successful, but at least they want to try.”
How has this journey changed the experience of the people in the hospital?
“Well, the first thing I have noticed is how much teamwork I have seen. It has brought the staff closer. It has brought them closer with the administration, just because we’re all working together on this That’s a huge positive to me. Also, providing this education and helping these moms I feel has helped these nurses connect more with these patients, where the patients feel more like they’re not just a number. This is a major experience and something that they will remember forever. We want this to be as enjoyable as we can make it. And seeing these babies, how healthy they’ve been, how alert, and how happy the moms have been – because they feel like they’ve been a part of their care. For a long time, it was just, ‘Here you go, here’s your baby.’ Somebody else had to teach them how to take care of them. But we teach them in the hospital…feeding, diaper changes, cleaning the umbilical cord, taking care of circumcision, all of that…even mixing formula…so that they know what to do when they get home. I’ve really seen a change in the education that they know coming in.”
How has this affected your community?
“We’re a very small hospital. We deliver about 300 babies a year. And it’s been a huge thing for our community. We’ve even talked about doing some group prenatal care – just to kind of get these community members to know each other, support each other at different times in their pregnancy. We would love to do that to improve the community in that way. Ultimately, if we can just help a few families, I feel like we’ve done more than nothing. I wish I could change the world, but I can change my county.”
Before and After Baby-Friendly: A Frontline Nurse’s Perspective
Jennifer Layton, RN

What is your role in the hospital?
“I see the moms when they come for check-ups throughout their pregnancy. They come in and have their tests, like if they have high blood pressure or history of miscarriage or anything, they come and get checked out early in their pregnancy. So, we do some teaching throughout that time in their pregnancy. We also see them as soon as they come in to get ready for delivery and throughout their postpartum care. We have 2 RNs on my shift, 3 RNs on the opposite shift on days, a couple of RNs at night. And then we also have aids in the nursery to help out with the process with the babies. So, we all kind of work as a team to help them.”
What are some of the challenges you face?
“Some moms in our area don’t have basic knowledge about what to expect. So, a lot of times, we have to instruct them and show them that just because you don’t have milk today, you do have a way of helping your child. With us all helping, it really does make a difference. And I have seen moms that come in, say, on Monday and they’ve delivered a baby and they absolutely do not want to breastfeed and the baby doesn’t feed well on formula. And by Wednesday when they go home, they’ll be strictly breastfeeding. So, we’ve actually had some really good outcomes with our teaching and our assistance with them.”
Why are you so committed to this?
“I am. In fact, next month I’m going to learn to be a clinical lactation counselor – because I’m so passionate about it and I would love to be able to help more. It has helped so much with so many people. I’ve enjoyed it so much that I want to be able to teach more.”
Can you say more about how this is helping people?
“Well, we have so many low birth weight children. And we see where we have these low birth weight children come in, they’re 5 or 6 pounds. And then they come back in at 6 weeks and the babies have gained weight and they’re 7 or 8 pounds. They come in at 6 months and they’re up to their target weight where they should be. They’re no longer in their low percentile weight and you can see they’re developmentally where they’re supposed to be. They’re doing fabulous. We just see so many where we started out thinking we’re going to have a problem baby and then they come back at 6 months and they’re fabulous.”
And you attribute that to the breastfeeding?
“I attribute that to the bonding with mom and the breastfeeding – to more nutrients and contact with mom. I just think that we see so many more thriving babies due to being able to breastfeed and being able to have this Baby-Friendly response. Before this, we had moms who went home and didn’t know anything about how to take care of the baby. But we’re rooming in now, and when they leave, they know more about how they actually have to take care of the baby. Before, we kept the baby in the nursery, they saw the baby a couple hours a day. Now the baby’s in the room and they learn so much more about how to take care of their own baby. We check on mom and baby and we can help her with how to hold the baby, how to feed the baby, make sure the baby sleeps in her crib in the room with you. When the baby wakes up in the middle of the night, when she’s doing this or doing that, we’re teaching mom how to take care of her baby and learn feeding cues. She learns when the baby wakes up and the baby is quiet but the baby is sucking on her hands, OK, this is the time to feed her, don’t wait till she wakes up crying. OK, your baby’s wet, let’s change the baby, let’s not wait until the baby’s screaming. All sorts of things. And we have a lot of 13, 14, 15 year-old moms some of them don’t think about, this baby’s going to cry, this baby’s going to need bottles and diapers.”
So how would that picture have looked 5 or 10 years ago?
“She would have had the baby. The baby would have gone to the nursery for 2 hours until we got it stable. We would have bathed the baby, took the baby out to mom for a little while. Mom would have gotten tired and ready to go to sleep, so she’d call the nursery. Nursery would have taken the baby back to the nursery so she could sleep. She would sleep all afternoon. When she got ready to see the baby, when friends came to visit, she’d get the baby, come back out and play with the baby for a little while. When she got tired and wanted to take a nap, and didn’t want to fool with the baby anymore, she’d call the nursery and baby would go back to the nursery and stay in the nursery till she got ready to play with it again and she’d take it back in there. Whenever the baby needed to be changed, she’d call the nursery – I need help. She didn’t have to do anything. The nursery did everything for her. So basically, she had a sitter for her baby and she just got to play with the baby.”
And now?
“Now she takes care of everything and we come in there and assist her with anything that she has questions about. Now we go in there and help her, but we let her learn how she takes care of her baby.”
It sounds like Baby-Friendly to you is much more about helping the mother be a good mother than it is about encouraging the mother to breastfeed. Is that correct?
“Yes, granted, breastfeeding is great for the baby, and yes, we do want them to breastfeed as much as we can get them to do. But even for the moms who don’t breastfeed, we want to help them take care of their babies and teach them the correct way of doing things. Especially for the younger moms who have no idea what they’re doing when they go home with the baby. I really feel like it’s helping them because they don’t come back as much with babies who are crying all the time. They don’t come back with ear infections all the time from laying on the bed and propping the bottle up – they don’t understand they can’t do that. They aren’t coming back with stomach problems because they’re overfeeding the baby too much – because we kept them from doing that in the hospital.”
Have you ever gotten any criticism that you’re pushing too hard for mothers to breastfeed?
“I think we were trying a little too hard at first and I think we did turn away some people because they were feeling pressured. But I don’t want to pressure anybody. I have figured out that it’s better just to educate and if somebody finds that they enjoy it then they will.”
And how do you think this will affect the community in the long-run?
“Down the road, I think we’re going to see a closer family, a closer-knit mother-child bond. We have grandmothers and extended families taking care of babies and moms don’t have the attachment with their babies. I think this will bring moms closer to their children. We’re going to see more maternal attachment and we’re going to see the family come back in our community. That’s what I feel.”
Before and After Baby-Friendly: A Mother’s Perspective
Tina Bennett

Can you tell us what happened after the birth of your first child?
“He was born at 6:45 pm and I didn’t get him until after midnight. They delivered him and cut the cord and everything and my husband brought him to me and let me see him. And after that, they took me to recovery. And I was so exhausted from the day that I was just kind of out of it. I remember waking up and asking to see my baby. And they brought him to me for a little while, but then they came back and got him.”
Did you attempt to breastfeed?
“I tried to a little bit when they first brought him to me and he wouldn’t latch. And so they offered a bottle and so I gave him a bottle. And I never really tried to nurse him anymore while I was at the hospital, although my intentions were to do that. I honestly hadn’t educated myself enough on breastfeeding and what it takes to do and what you need to do and what you don’t need to do. And so, I never tried to latch him again at the hospital. I did try to latch him again at home, and I never could get him to latch well.”
Did you keep trying to give him breast milk?
“Yes, I did pump some after I got home – and again, I didn’t educate myself enough on what I needed to do to pump to keep my supply up for him. And so, I never gave him strictly breastmilk during the daytime. He got whatever I was able to pump plus formula because I wasn’t pumping like I should have been had I wanted to pump and feed. And so, I pumped for six weeks, but he never got more than one or two breastmilk bottles a day and he didn’t get a whole lot of breastmilk. And after I went back to work – because I was only producing a half an ounce to an ounce at a time – I just didn’t even fool with trying to pump anymore at that point.”
How was your second birth different from the first?
“From day one, every time I went for a prenatal appointment, they gave me hand-outs about breastfeeding and Baby-Friendly and they talked about it. The nurses came in and said, you know we’re Baby-Friendly now. This is how it works. This baby doesn’t really leave your room. We don’t have a real baby nursery anymore. It’s there in the event that you cannot care for your baby, but if you’re able to care for your baby, he’ll be with you from the moment he’s born. They also talked about skin-to-skin and how important skin-to-skin is and talked about breastfeeding and what to expect and what not to expect, breastfeeding versus formula feeding. Different things like that they gave me throughout my nine months of seeing them every month. So, I knew what to expect – versus with my first, I said, breastfeeding is natural, let’s go in, I’m going to have a baby and it’s going to breastfeed.”
Your second birth was a planned c-section. How long were you apart from your baby this time?
“I would say no longer than 30 minutes. We did the delayed cord cutting for the first minute. And then they took him and did his Apgar test and my husband had him while I was getting sewed up and everything. And then after they sewed me up, they brought me to recovery, where my husband was waiting for me and they put him directly on my chest. And he stayed on my chest until his temperature got up to normal and he stayed there for a little while. And then they came into the room and got him and bathed him in my room and he never left my room from that time at all, except for the circumcision.”
And how was the breastfeeding experience different?
“He tried to feed some while in recovery, but not a whole lot. But after we got back to the room, while he was still doing skin-to-skin, he did get on my breast real quickly after that and never had any trouble latching.”
And he’s been breastfeeding successfully ever since?
“Yes. I’ve had no issues. He’s had no formula.”
Can you give us your reflections on the experience?
“I really loved it the second time because I didn’t have to worry about what was going on when he was away from me – because he was never away from me. I really liked that. I was also more educated on what to expect when it came to breastfeeding and I really wanted to breastfeed. So, I felt more comfortable doing it from the get-go. I never had a nurse offer me a bottle either because they knew I was breastfeeding, so they never even offered me a bottle. I knew that if I needed one, they would give me one, but they never offered it to me.”
Before and After Baby-Friendly: A Mother’s Perspective
Tiesha Lee

How did you come to breastfeed your second child when your first child was formula fed?
“When I had my son, no one mentioned breastfeeding. I wasn’t aware of breastfeeding. It was like I was in the dark about that. When I had my daughter, they asked me if I wanted to breastfeed and I was introduced to all the benefits and everything dealing with breastfeeding.”
How were you introduced to the benefits?
“After I had her, they asked me, did I want to try it. I was like, no, I don’t want to try it. I wanted to bottle feed, but she didn’t take to the bottle. We tried for two days to get her to take the bottle, but she wouldn’t take it. So that’s how I ended up breastfeeding. Everything I needed to know about breastfeeding, they helped me 100 percent during that and I began to get used to it. It was something I didn’t want to do, because I never had done it. But I’m glad I did it because there’s a lot of benefits from it. And it’s way different from when I had my son than when I had my daughter.”
What do you see as the benefits?
“The benefits I see of breastfeeding are, my daughter has barely been sick. And she’s really smart. She’s two. She knows her colors and shapes and animals. She knows her birthday. There’s a lot of things I see different from breastfeeding because my son was bottle feed. She had an ear infection, I give her the breastmilk and the breastmilk clears up the ear infection. Same with her colds. It has a lot of benefits for her and I’m glad I went that route with her.”
But you hadn’t started out thinking you would breastfeed?
“No, I didn’t want to breastfeed. When I was pregnant, everyone kept asking me and every time they asked me I said no. But it ended up I had to do it anyways and I’m glad that I did it.”
Why were you opposed to the idea originally?
“Because I had never done it before and I was listening to other people and I was basically going on ‘he said, she said’ and I was like, no, I’m not going to try this for myself. And besides, I never tried it, so that’s what made me not want to do it.”
Do you remember if they put your daughter on your chest skin-to-skin right after birth?
“Yes, we had skin-to-skin contact right after she was born.”
How did you like that?
It was a great feeling because I didn’t feel that with my son. They didn’t do skin-to-skin when my son was born. So, it felt wonderful to be able to have skin-to-skin contact with her after she came out.
Do you think it helped you bond with her?
Yes, it did. It helped me bond with her a whole lot. Especially with this breastfeeding journey, it helped me bond with her even more than the skin-to-skin. So, we have a great bond that’s amazing that I love with her. I enjoy it a whole lot.
Did you notice differences in the procedures after each birth?
Well, they were born in two different hospitals. When my first child was born, breastfeeding was not then promoted as it is now, so I didn’t know anything about breastfeeding. I wish I could have, but I didn’t at the time. I was young and I wasn’t paying attention to it then. But when I had my daughter, everything was promoted – skin-to-skin, breastfeeding and everything.
You started out wanting to give your daughter formula. What changed?
She was crying a lot and I asked if someone could please bring me a bottle. And they said, why don’t you try your breast first. I said, no, I don’t want to breastfeed. So, they brought the bottle to me, but she wouldn’t take it. For two days, she wouldn’t take it. So, they said again, why don’t you try your breast. The moment I tried it, she latched on, no problem. It’s like she knew what she wanted anyway. What I wanted for her she didn’t want, but she knew what she wanted.
And you think it has made her a healthier child?
Yes, definitely. Healthier and smarter. She is exclusively breastfed. It makes a big difference, breastfeeding. And I promote it also. I think breastfeeding is the reason she is the way she is.